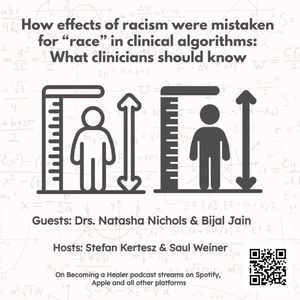
How effects of racism were mistaken for “race” in clinical algorithms: What clinicians should know
12/19/23 • 63 min
For years, when physicians order tests to assess lung function, or blood work to determine kidney function, or look up guidelines for managing high blood pressure the results have been adjusted for race. This practice has been based on studies that seemed to indicate that the same result means different things if the patient is Black vs white. So, for instance, an “uncorrected’ creatinine of 1.6 was thought to be less concerning in a Black than white patient as Blacks were thought to have greater muscle mass (not true). These correction factors masked underlying environmental and social stressors disproportionately affecting Black Americans. Regrettably they also contributed to delays in care for chronic conditions, as Black patients had to be sicker than white patients to trigger therapeutic interventions – further exacerbating disparities. We talk with two physicians who lead an anti-racism equity committee based in a Chicago VA hospital to understand the history and science that led to these “corrections,” and how they have successfully been removing them through education and advocacy across their organization and nationally. Their activism is especially meaningful because of its immediate, tangible, benefit for affected patients. The views expressed in this episode are those of the participants and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
For years, when physicians order tests to assess lung function, or blood work to determine kidney function, or look up guidelines for managing high blood pressure the results have been adjusted for race. This practice has been based on studies that seemed to indicate that the same result means different things if the patient is Black vs white. So, for instance, an “uncorrected’ creatinine of 1.6 was thought to be less concerning in a Black than white patient as Blacks were thought to have greater muscle mass (not true). These correction factors masked underlying environmental and social stressors disproportionately affecting Black Americans. Regrettably they also contributed to delays in care for chronic conditions, as Black patients had to be sicker than white patients to trigger therapeutic interventions – further exacerbating disparities. We talk with two physicians who lead an anti-racism equity committee based in a Chicago VA hospital to understand the history and science that led to these “corrections,” and how they have successfully been removing them through education and advocacy across their organization and nationally. Their activism is especially meaningful because of its immediate, tangible, benefit for affected patients. The views expressed in this episode are those of the participants and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Previous Episode
Drug testing at time of birth: How physicians are co-opted into harming families while thinking they are doing the right thing
The practice of urine drug testing during pregnancy and then often reporting positive results to Child Protective Services triggers a cascade that can result in separation of mother and newborn, with devastating consequence for both. These practices are more common when patients come from marginalized communities even when baseline substance use rates are the same. As our guest -- obstetrician/gynecologist and addiction medicine expert Mishka Terplan MD, MPH -- points out, illicit substances are not teratogens in comparison to, say, alcohol, tobacco or lead exposure. So why do we order these tests? He also discusses how talking with patients about substance use behaviors, especially with the help of screening instruments, is the only way to characterize substance use behaviors and formulate treatment strategies.
This is the third episode in which we learn of common clinician practices in which clinicians are co-opted into punitive and even carceral systems of oppression.
Next Episode
About me being racist: A conversation that follows an apology
We are re-running this episode from 2021 because we’re releasing a sequel next month in which Saul reflects on his journey confronting racist ideas he’d absorbed and that became impossible to ignore after he’d acknowledged his role in the incident described here. We are also re-running the episode because it exemplifies our commitment to facing things -- about ourselves and our profession – to enhance our wellbeing, and our relationships with colleagues and patients. Rather than disheartening, we find such conversations and the changes they bring rewarding and healing.
If you like this episode you’ll love
Episode Comments
Generate a badge
Get a badge for your website that links back to this episode
<a href="https://goodpods.com/podcasts/on-becoming-a-healer-505861/how-effects-of-racism-were-mistaken-for-race-in-clinical-algorithms-wh-66499646"> <img src="https://storage.googleapis.com/goodpods-images-bucket/badges/generic-badge-1.svg" alt="listen to how effects of racism were mistaken for “race” in clinical algorithms: what clinicians should know on goodpods" style="width: 225px" /> </a>
Copy